ANKYLOSING SPONDYLITIS
Delving Into the Complexities of a joint inflammation.
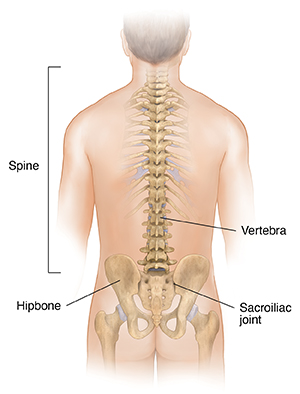
The word “Ankylosing” means stiff or rigid and “Spondyl” means spine. Ankylosing Spondylitis refers to a long-term inflammatory condition affecting the mainly the joints and ligaments of the spine, and sometimes peripheral joints like hips, knees and ankles.
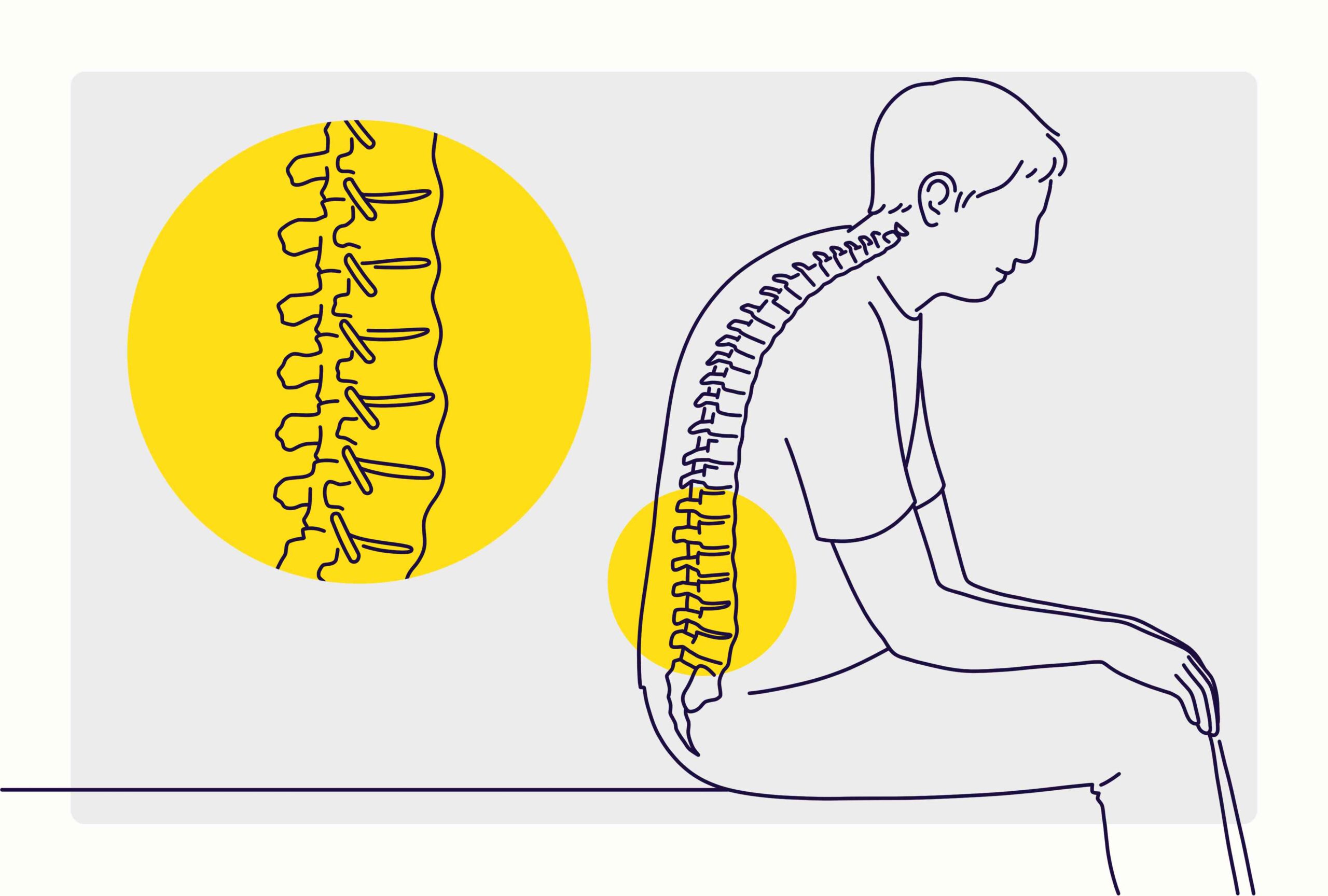
As a consequence of the inflammation, the body generates additional calcium in the vicinity of the vertebral bones. This may result in additional bone growth and stiffness in the back and neck. On rare occasions, the excess calcium may cause some of the bones in the vertebrae to fuse or connect. Serious cases may result in an increased forward curvature of the vertebrae and make the individual bend forward.
AS is more prevalent among individuals aged 17 to 35. It can also manifest in elderly individuals and infants. Young males are more susceptible to the disease than women. It is commonly inherited and runs in families (1).
Symptoms of Ankylosing Spondylitis
- Lower Back Pain: Frequently manifesting as dull discomfort and stiffness in the pelvis and lower back. It is particularly noticeable when one awakens after periods of inactivity.
- Sacroiliitis: Sacroiliitis is an inflammatory condition characterized by discomfort in the lower back or buttocks, which may also extend down the legs.
- Spinal Stiffness: It is characterized by severe impaired mobility, especially upon awakening or following periods of inactivity.
- Progressive Spinal Fusion: As the inflammation of the vertebrae progresses, it can result in their fusion, which manifests as a deformed and rigid spine.
- Peripheral Arthritis: It’s the condition where the hips, knees, and shoulders are affected, albeit to a lesser extent than symptoms observed in the axial region.
-
- Uveitis: An inflammation of the eye characterized by pain, irritation, and impaired vision.
- Cardiovascular Issues: Aortitis, dysfunction of the cardiac valves, and conduction abnormalities are all potential cardiovascular complications.
- Involvement of The Intestines: Certain patients may exhibit subclinical inflammation of the intestines.
- As well as Fatigue, loss of appetite, and weight reduction.
How is Ankylosing Spondylitis Diagnosed?
Initially, a family and medical history along with a physical exam are conducted by the physician to diagnose Ankylosing Spondylitis. Additional tests may be ordered, such as:
- X-ray
- MRI
- Mobility Tests (3, 4)
- Genetic testing
- Erythrocyte sedimentation rate (ESR or sed rate)
What are the causes of Ankylosing Spondylitis?
- Researchers are still working to fully understand the exact process by which Ankylosing Spondylitis (AS) develops. However, they hypothesize that it arises from a complex interplay between genetic, immunological, and environmental factors.
-
In the majority of white Americans with Ankylosing Spondylitis, a gene known as HLA-B27 is present. 50% of African Americans with Ankylosing Spondylitis, however, carry this trait. Additionally, certain individuals harboring the HLA-B27 gene do not manifest Ankylosing Spondylitis. With the HLA-B27 gene, less than 5% of individuals have Ankylosing Spondylitis. Moreover, 80% of offspring who inherit the mutated gene from a parent with Ankylosing Spondylitis do not, in fact, develop the disorder (5).
How is Ankylosing Spondylitis treated?
The goal of treatment is to alleviate pain and stiffness while also preventing or postponing consequences including spinal deformity. Treatment for ankylosing spondylitis is most effective before the disease causes irreversible damage.
The medications used are:
- Nonsteroidal Anti-Inflammatory Drugs (NSAIDs): NSAIDs like ibuprofen or naproxen to control pain and inflammation
- Disease-Modifying Anti-Rheumatic Drugs (DMARDs): Sulfasalazine if peripheral joints are affected
- TNF inhibitors IL-17 inhibitors: prescribed for patients who don’t respond to traditional therapies.
- Short-term use of muscle relaxants and pain relievers
- Short-term use of corticosteroids, to relieve inflammation
Besides medications, physicians also prescribe Exercise regimen, particularly those focused on spinal flexibility and posture, and lifestyle modification by ceasing smoking, and reducing weight for managing Ankylosing Spondylitis.
In severe cases, Joint Replacement surgery or arthroplasty may be conducted when the hip or knees are affected. Rarely, spinal surgeries like osteotomy may be performed to correct severe deformities (4, 6)
Believe you have symptoms of Arachnoiditis?
Contact Longhorn Brain & Spine
Bibliography
- Braun J, Sieper J. Ankylosing spondylitis. The Lancet. 2007;369(9570):1379-90.
- Sieper J, Rudwaleit M, Baraliakos X, Brandt J, Braun J, Burgos-Vargas R, et al. The Assessment of SpondyloArthritis international Society (ASAS) handbook: a guide to assess spondyloarthritis. Annals of the rheumatic diseases. 2009;68(Suppl 2):ii1-ii44.
- Van Der Heijde D, Ramiro S, Landewé R, Baraliakos X, Van den Bosch F, Sepriano A, et al. 2016 update of the ASAS-EULAR management recommendations for axial spondyloarthritis. Annals of the rheumatic diseases. 2017;76(6):978-91.
- Rademacher J, Poddubnyy D. Emerging drugs for the treatment of axial spondyloarthritis. Expert Opinion on Emerging Drugs. 2018;23(1):83-96.
- Brown MA, Kennedy LG, Macgregor AJ, Darke C, Duncan E, Shatford JL, et al. Susceptibility to ankylosing spondylitis in twins the role of genes, HLA, and the environment. Arthritis & Rheumatism. 1997;40(10):1823-8.
- Khan MA. Update on spondyloarthropathies. Annals of internal medicine. 2002;136(12):896-907.