MINIMALLY INVASIVE TLIF
What’s Minimally Invasive TLIF?
Minimally Invasive Transforaminal Interbody Fusion refers to a variation of a similar surgery; posterior lumbar interbody fusion, often performed as a surgical procedure that requires minimal incision (as the name implies- minimally invasive). For the sake of brevity, spinal specialists usually refer to this surgery in its shorter term; “MIS TLIF”. This surgical procedure aims to relieve back ache, pain from the leg caused by degeneration of discs, spinal stenosis and spinal instability.
Spinal stability procedure involves entry into the vertebral (lumbar) foramina via two methods: Either through the conventional open surgical approach (where a larger incision ought to cut at the middle of the back), or through minimally invasive surgical (MIS) approach. During the MIS procedure, the surgeon makes two small incisions on each side of the back (paramedian incisions) and special surgical tools, known as expandable tubular retractors, provide access to the spine without serious disruption of the muscle tissue. For easy visualization, the surgeon uses an endoscope.
Conditions that TLIF surgery treats:
TLIF is a surgical procedure performed to address specific conditions affecting the lumbar spine. It is typically recommended for patients who display indicators such as:
1. Degenerative Disc Disease: TLIF may be used when discs in the lumbar spine become worn out or damaged, leading to pain, instability, and nerve compression.
2. Spinal Stenosis: It is often considered for patients with spinal stenosis, a condition where the spinal canal narrows, exerting pressure on the spinal cord or nerves.
3. Spondylolisthesis: TLIF might be recommended to individuals with spondylolisthesis, which occurs when one vertebra slips forward or backward over the adjacent vertebra, causing instability and nerve compression.
4. Herniated Discs: It could be an option for patients whose herniated discs in the lumbar spine are causing persistent pain, weakness, or numbness due to nerve compression.
5. Failed Back Surgery Syndrome: It may be considered for patients who have experienced inadequate relief or recurrent symptoms after previous back surgery.
6. Unstable Spine: TLIF can stabilize the spine by fusing two vertebrae together, providing stability and reducing pain in patients with spinal instability due to trauma or other conditions.
Surgical procedure
This surgery takes approximately 1 to 2 hours or even more. This depends on how many vertebral bodies the surgeon has to fuse. Minimally Invasive TLIF requires a number of procedures, prior to the surgery and post-surgery.
- Prior to the surgery, the anesthesiologist will bring the patient to the operating room and put the patient to sleep before the operation. The anesthesiologist administers general anesthesia, this ensures the patient remains unconscious throughout the period of the surgery.
- Two qualified nurses provide assistance for the performing surgeon, along with a surgical assistant. These health personnels help to reduce the workload on the surgeon, by providing the necessary surgical tools and professional assistance when required.
- To begin the surgery, the surgeon makes one or two small incisions on either side of the patient’s back. The length of these incisions depends on the number of vertebral levels that require fusion. If fusion must occur at two or more vertebral levels, the length may increase.
- Special retractors (expandable or non-expandable retractors) come into use. Placement of these retractors helps to expose the posterior aspect of the spine with minimum disruption of muscular tissue.
- The next procedure involves removal of a small amount of bone and ligament(s) exerting pressure on the spinal canal.
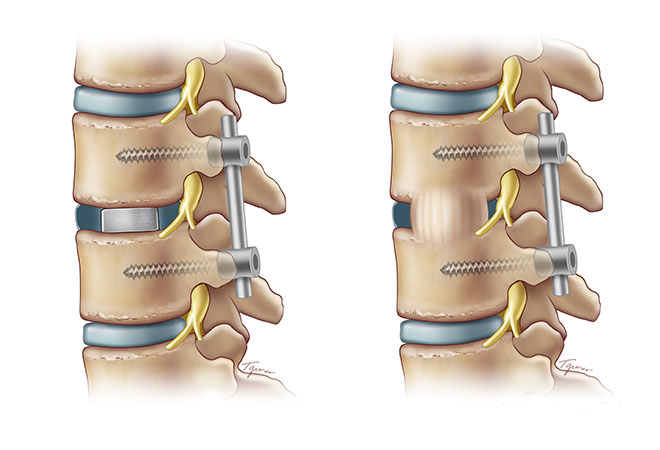
- The surgeon then removes the painful disc with special instruments and replaces it with a fusion device. This fusion device consists of a titanium box, filled with bone graft material.
- Following replacement of the painful disc, placement of titanium screws and rods into the bones above and below the disc takes place. With the aid of x-ray guidance, the surgeon places the rods and screws through the small incisions made earlier. These tools aim to increase stability, which helps the fusion, heal.
- To close the incision, the surgeon uses resorbable stitches placed beneath the skin.
Risks of TLIF surgery Spinal fusion is a high-risk surgery with serious complications, including death. There is a higher risk of complications in older people with elevated body mass index (BMI), other medical problems, poor nutrition and nerve symptoms (numbness, weakness, bowel/bladder issues) before surgery. Complications of TLIF surgery Like any surgery, complications may include infection, blood loss, and nerve damage. Fusion also changes the normal motion of the spine and results in more stress on the vertebrae above and below the fused segments. As a result, long-term complications include degeneration at these adjacent spine segments.
How long does it take to recover from a TLIF procedure?
Recovery from TLIF surgery Recovery following spinal fusion is extremely variable, it ranges from 6 to 12 weeks, although it varies from patient to patient. Recovery typically involves both restriction of certain activities and rehabilitation training. Restrictions following surgery largely depend on surgeon preference. A typical timeline for common restrictions after a lumbar fusion surgery are listed below: • Activity Restriction: Avoid high impact activities, heavy lifting, and repetitive tasks that require range of motion in the lower back for at least the first six weeks after surgery. This means any tasks that involve bending, lifting, and twisting of the lumbar spine.
Patients typically undergo x-ray imaging again to get flexion (bending to touch the toes) and extension (leaning back at the waist) views of the lumbar spine. These check spinal range of motion and confirm that there is no vertebral sliding because of the implant. All patients are back at work and performing a normal routine. The incision is well healed.
References
Jeffords, P (2022). Minimally invasive TLIF (https://www.pauljeffordsmd.com/minimally-invasive-surgical-mis-tlif)
