Guillain-Barre Syndrome
Delving Into the Complexities of a Neurological Condition
Guillain-Barré Syndrome (GBS): An Overview
Characterized by a swift onset of symptoms, GBS typically shows signs with tingling or weakness in the lower extremities and progress upwards. GBS can affect individuals of all ages, with a higher prevalence in males and adults over the age of 50. In the United States, GBS afflicts between 3,000 and 6,000 people each year (1, 2).
Symptoms of Guillain-Barré Syndrome
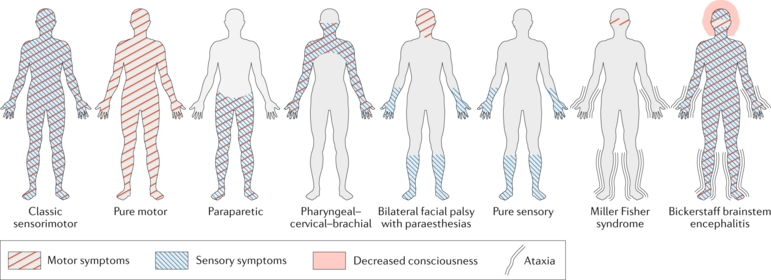
Guillain-Barré syndrome presents a range of symptoms and typically follows a course lasting several weeks. Key symptoms of Guillain-Barré syndrome include:
- Weakness or Tingling Sensations: Often beginning in the legs and progressing to affect the arms and face. In some cases, they can lead to paralysis of the legs, arms, or facial muscles. Additionally, about one-third of patients also experience compromised chest muscle function.
- Difficulties with Speaking and Swallowing: In severe cases, these symptoms can become life-threatening, necessitating intensive care unit treatment.
- Rare and Adverse Complications: In exceptional circumstances, a small fraction of Guillain-Barré syndrome patients may face life-threatening complications, including respiratory muscle paralysis, blood infections, pulmonary embolism (lung clots), or cardiac arrest.
Additional symptoms associated with Guillain-Barré syndrome encompass:
- Double Vision or Inability to Move the Eyes: These vision-related issues can occur.
- Challenges with Bladder Control or Bowel Function: Some individuals may experience difficulties in these areas.
- Elevated Heart Rate: The heart rate may become rapid.
- Abnormal Blood Pressure Levels: Blood pressure can either drop significantly (low) or rise (high).
- Impaired Ability to Walk or Climb Stairs: Mobility issues, such as difficulty walking or climbing stairs, can also be observed in some cases.
It’s important to note that Guillain-Barré syndrome is a rare condition, and while it can be serious, many individuals do recover with appropriate medical care (1, 2).
Diagnosis of GBS
Diagnosis of GBS typically commences with a comprehensive clinical assessment by a healthcare provider involving a detailed review of the patient’s medical history, symptom inquiry, and a physical examination.
- Cerebrospinal Fluid Analysis (Lumbar Puncture): In GBS, a distinctive marker known as “albuminocytologic dissociation” is identifiable. This refers to an elevated protein level in the cerebrospinal fluid (CSF) without a concurrent increase in white blood cells. It serves as a hallmark of GBS and aids in confirming the diagnosis.
- Electrophysiological Investigations: Healthcare providers frequently perform nerve conduction studies, measuring nerve conduction velocity, and electromyography (EMG). These tests aid in distinguishing various GBS variants and provide insights into the severity and distribution of nerve involvement. GBS typically exhibits characteristic patterns of nerve damage.
- Blood tests: Healthcare providers conduct blood examinations to rule out alternative conditions and explore potential triggers of GBS, including infections. This aids in the diagnostic process by eliminating other conditions with similar symptoms.
- Pulmonary Function Examinations: For severe GBS cases, there is a risk of respiratory failure due to muscle weakness affecting the chest muscles and diaphragm. Pulmonary function tests may be conducted to assess respiratory muscle strength and determine the need for respiratory support.
- Additional diagnostic tools: While not always necessary, healthcare providers may employ imaging studies like MRI or CT scans. These tests help rule out conditions that might resemble GBS or provide insights into nerve and muscle involvement, further confirming the absence of other underlying issues.
The diagnosis of GBS relies on the combination of clinical presentation, cerebrospinal fluid analysis, and electrophysiological testing. Once GBS is diagnosed, treatment can be initiated promptly to manage symptoms and prevent complications. Early diagnosis and intervention are crucial for a better prognosis in GBS cases.

What causes Guillain-Barré Syndrome (GBS)?
The precise cause of Guillain-Barré Syndrome (GBS) remains elusive, but it is generally believed to be associated with autoimmune reactions and is often triggered by infections. Some of the causes are described below:
- Vaccinations: Although rare, reported cases of GBS have been linked to certain vaccines, including the influenza vaccine and those targeting diseases such as the flu.
- Infections: GBS often follows viral or bacterial infections. Notable infections associated with GBS include:
- Campylobacter jejuni: This bacterium, often acquired from undercooked poultry, is a primary antecedent to GBS.
- Influenza (Flu) and Other Viral Infections: GBS can occur after respiratory infections, such as the flu, as well as other viral infections like cytomegalovirus, Epstein-Barr virus, or the Zika virus.
- Surgical Procedures: GBS has been observed following surgical operations, although the exact reasons for this association are not fully understood.
- Genetic Predisposition: Some individuals may have a genetic predisposition that makes them more susceptible to developing GBS, increasing the risk in specific cases.
- Underlying medical conditions: Hodgkin’s lymphoma or autoimmune diseases like lupus can trigger GBS. It’s important to note that while these conditions are not direct causes of GBS, they can be associated with the syndrome.
It’s crucial to recognize that GBS remains a multifaceted and relatively uncommon condition with various contributing factors. Understanding these associations holds significance in both the diagnosis and management of the syndrome.
How do medical professionals treat Guillain-Barré Syndrome (GBS)?
Although there is no direct treatment for Guillain-Barré Syndrome (GBS), healthcare providers frequently employ two fundamental techniques to modulate the immune response: intravenous immunoglobulin (IVIG) and plasma exchange (plasmapheresis).
-
- Intravenous Immunoglobulin (IVIG): The intravenous administration of immunoglobulin G (IgG) derived from a pool of donors. While the precise mechanism of its effectiveness remains unknown, medical experts believe that IVIG neutralizes pathogenic antibodies and suppresses inflammatory reactions. Furthermore, IVIG is generally as effective as plasmapheresis but has the advantage of easier administration.
- Plasma Exchange (Plasmapheresis): Involves the removal of plasma containing antibodies from the blood and its replacement with a substitute fluid. The primary objective is to eliminate autoantibodies contributing to the disease process.
Other treatments can involve:
-
- Supportive Care: Patients who experience respiratory failure may require mechanical ventilation.
- Pain Management: Healthcare providers use medications like antiepileptics and opioids to address neuropathic pain.
- Physical Therapy: Vital for enhancing long-term outcomes, especially in terms of muscle strength and functional ability.
- Follow-Up and Monitoring: Regular monitoring is essential to track disease progression, assess respiratory function, and detect any medication-related side effects (1, 6)
Believe you have symptoms of Guillain-Barré Syndrome?
Contact Longhorn Brain & Spine
Bibliography
- Van den Berg B, Walgaard C, Drenthen J, Fokke C, Jacobs BC, Van Doorn PA. Guillain–Barré syndrome: pathogenesis, diagnosis, treatment and prognosis. Nature Reviews Neurology. 2014;10(8):469-82.
- Wijdicks EF, Klein CJ, editors. Guillain-barré syndrome. Mayo clinic proceedings; 2017: Elsevier.
- Durand M-C, Porcher R, Orlikowski D, Aboab J, Devaux C, Clair B, et al. Clinical and electrophysiological predictors of respiratory failure in Guillain-Barré syndrome: a prospective study. The Lancet Neurology. 2006;5(12):1021-8.
- Nachamkin I, Allos BM, Ho T. Campylobacter species and Guillain-Barre syndrome. Clinical microbiology reviews. 1998;11(3):555-67.
- Geleijns K, Schreuder GT, Jacobs B, Sintnicolaas K, van Koningsveld R, Meulstee J, et al. HLA class II alleles are not a general susceptibility factor in Guillain–Barré syndrome. Neurology. 2005;64(1):44-9.
- Hughes RA, Swan AV, Van Doorn PA. Intravenous immunoglobulin for Guillain‐Barré syndrome. Cochrane Database of Systematic Reviews. 2014(9).
