Extreme Lateral Interbody Fusion (XLIF)
Spinal disorders – debilitating conditions that constitute a major burden to sufferers, family members, and the healthcare system. Different medical and surgical procedures occur to manage this burden. This includes the Extreme Lateral Interbody Fusion (XLIF), an advanced surgical procedure, which can effectively treat these conditions.
XLIF
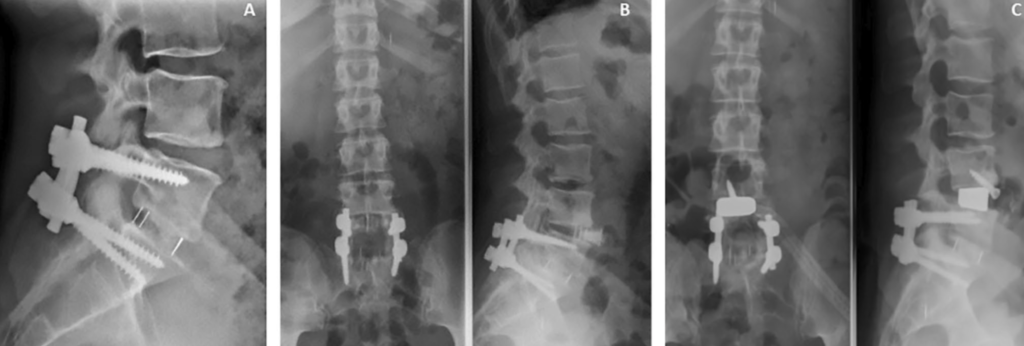
An innovative and minimally invasive surgical procedure used to treat spine disorders. This procedure involves accessing the patient’s spine from the side to remove a damaged disc nucleus, replacing it with a biocompatible polymer implant or a bone graft, and then allowing it to fuse.
Indications for XLIF
Due to the numerous benefits of this procedure, the indications for XLIF have broadened to include:
- Arthritis – a condition characterized by swelling and tenderness of one or more joints caused by inflammation in the joint.
- Bulging disc – a common spine injury that frequently affects the intervertebral disc. This condition develops when the outer shell of the disc weakens, causing the disc to bulge or flatten to one side of the spinal canal.
- Degenerative disc disease – an age-related condition that happens when one or more discs between the vertebrae of the spinal column break down and cause pain.
- Facet arthritis – a degenerative disease characterized by the wearing out of cartilage lining facet joints.
- Low back pain – also called lumbago, a common condition that affects the muscles, nerves, and bones of the back, between the bottom border of the ribcage and the lower fold of the buttocks. Pain can range from a faint aching to a strong stabbing sensation.
- Spinal deformities – spinal deformity generally refers to an abnormal curvature of the spine.
- Spinal fractures – a fracture involving the vertebrae.
- Spondylolisthesis – a spinal condition that causes pain in the lower back due to abnormal displacement of vertebrae.
- Spondylosis – a degenerative disease of the spine and intervertebral discs which can impact the mobility of the spine and affect the nerves.
- Spinal stenosis – a condition where the space around the spinal column begins to tighten, which can cause pressure that pinches the spinal nerve.
- Lordosis – an abnormal inward curvature of the lower spine.
- Myelopathy – a condition in which the spinal cord gets injured due to severe compression which occurs as a result of spinal stenosis, disc degeneration, disc herniation, autoimmune disorders, or other trauma.
- Failed back syndrome – spinal pain of unknown origin either persisting despite surgical procedures or appearing after surgical intervention for spinal pain originally in the same location.
Other indications include non-union, neurogenic claudication, and radiculopathies.
Benefits of XLIF
The introduction of XLIF procedure has advanced the surgical approach in the management of many spine diseases, some of its benefits over ALIF (Anterior lumbar interbody fusion), PLIF (Posterior lumbar interbody fusion), and TLIF (Transforaminal lumbar interbody fusion) include;
- Minimal pain during and after surgery – The XLIF procedure guarantees minimal disruption of sensitive muscles, ligaments, and bones, this reduces the intraoperative and postoperative pain associated with traditional spine surgeries.
- Reduced blood loss and scarring – involves making a small incision to assess the spine in this procedure, it ensures minimal bleeding and scarring of tissues.
- Decreased surgery time and hospital stay – a quick procedure (the average duration doesn’t last more than two hours).
- Lower infection rate – due to its minimally invasive nature, XLIF has a reduced risk of postoperative infections, making it a very safe procedure.
- Quicker return to daily life – shorter recovery period and this ensures a faster return to daily activities.
Steps in the XLIF procedure
•Done under general anesthesia and it starts by positioning the patient laterally on an appropriate surgical table with sufficient padding and draping.
•The Neurosurgeon makes a small incision (2-3cm) on the side of the patient’s body.
•Then a dillator to direct the path to the affected disc space and advanced monitoring helps to prevent damage to surrounding vessels and nerves, this ensures minimal contact to the psoas muscle and neurovascular structures.
•The Neurosurgeon uses a retractor to hold the incision open, providing easy visibility and access to the discs.
•Then removal of the diseased disc and an appropriate implant placed into the disc space to restore structure and provide mechanical support.
•Following placement of the interbody device, the Neurosurgeon removes the tubular retractor and closes the incision with a few stitches and sterile dressing.
•Bone grows within the vertebral bodies during the fusion period and the segment stabilizes when healing occurs.
•Internal fixation with pedicle or facet screws and plates may prove useful in order to act as a stabilization device or internal brace which holds the implant during the fusion period.
Complications of XLIF
Although a pretty safe and quick surgery, certain complications may occur with XLIF procedures, these include:
•Failure of spinal fusion to occur.
•Damage to the spinal cord.
•Damage to nerve and blood vessels.
•Infections.
•Pneumonia.
•Stroke.
•Urinary tract infections.
Recovery
The procedure has a very short recovery period, with patients fit for discharge within 24-72 hours of surgery. Complete recovery takes a few months, which is remarkable when compared to other traditional procedures that take over 6months. Good postoperative care and proper rehabilitation can further shorten the recovery period.
References
•Epstein, N.E. (2019, December 6). Review of Risks and Complications of Extreme Lateral Interbody Fusion (XLIF). (https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6911674/). Accessed 2022, August 18.
•Billinghurst J. Akbarnia B.A. (2009, June). Extreme lateral interbody fusion – XLIF.
(https://www.researchgate.net/publication/232107724_Extreme_lateral_interbody_fusion_-_XLIF). Accessed 2022, August 17.
•Global Spine Journals. (2017, March 24). How Safe is the XLIF Approach for a Skilled Surgeon When He Starts to Perform It
(https://journals.sagepub.com/doi/abs/10.1055/s-0036-1583018). Accessed 2022, August 18.
